Presented on behalf of all MATTERHORN (FGCL-4592-082) study investigators
Introduction: For patients (pts) with LR-MDS, anemia poses a major clinical challenge, with limited response to first-line erythropoietin (EPO)-stimulating agents (ESAs) and a median duration of response ≤2 years. Further, pts with RBC transfusion dependence (≥2 packed RBC [pRBC] units every 8 weeks [Q8W]) are less likely to respond to ESAs. Anemia treatments with novel mechanisms of action enabling transfusion independence (TI) are needed to reduce frequent RBC transfusion burden. Roxadustat is a first-in-class, hypoxia-inducible factor prolyl hydroxylase inhibitor for treatment of anemia with chronic kidney disease. In the MATTERHORN (NCT03263091) dose-selection stage, roxadustat was well-tolerated, and 37.5% of pts (9/24) with LR-MDS and low RBC transfusion burden ([LTB] 1 pRBC unit Q8W for two consecutive 8-week periods or 2-4 pRBC units Q8W) achieved TI. In the MATTERHORN double-blind stage, TI response rate and safety of roxadustat were further assessed.
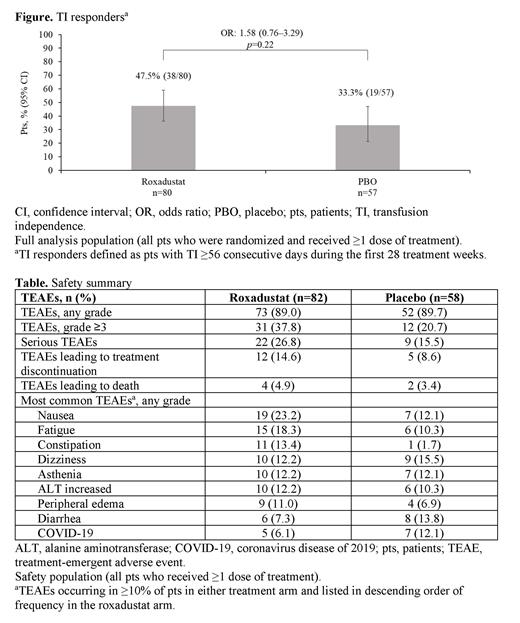
Methods: MATTERHORN is an ongoing, double-blind, Phase III, randomized, placebo (PBO)-controlled trial. Eligible adult pts (≥18 years of age) had very low-, low-, or intermediate-risk primary MDS per Revised International Prognostic Scoring System (IPSS-R) classification (<5% bone marrow blasts); hemoglobin (Hb) ≤10.0 g/dL at baseline (BL); and LTB. Prior ESA use (>8 weeks before randomization) was permitted. Pts were randomized 3:2 to roxadustat or PBO, then stratified by serum EPO concentration (≤200 or 200-400 mIU/mL), IPSS-R risk, and transfusion burden. Pts received oral roxadustat (starting dosage: 2.5 mg/kg three times weekly based on the dose-selection stage) or PBO with best supportive care (BSC; per institutional criteria, including RBC transfusion) for a 52-week treatment period, followed by a 4-week follow-up period. Primary efficacy endpoint was percentage of pts with TI (the absence of RBC transfusion) for ≥56 consecutive days during the first 28 treatment weeks (TI responder). The percentage of pts with TI and mean Hb increase of ≥1.0 and ≥1.5 g/dL (averaged over 8 weeks) compared with BL pretransfusion Hb was also assessed (to be reported separately). Safety (including treatment-emergent adverse events [TEAEs] and serious TEAEs) was evaluated throughout the study.
Results: As of the final 28-week interim analysis of the double-blind stage (data cutoff: April 24, 2023), 140 pts (82 roxadustat, 58 PBO) were randomized and treated. Across arms, median age was 71.5 years (range, 26-96), 59.3% (83/140) were male, and 80.0% (112/140) were white. Most pts (72.1% [101/140]) had IPSS-R low-risk disease and a transfusion burden of 2-4 pRBC units Q8W (92.1% [129/140]). Median (range) BL transfusion burden was 2.5 (1-10) pRBC units. Seventy pts (50.0%) received prior ESAs (98.6% [69/70] were ESA-refractory). Eighty-four pts (41/82 [50.0%] roxadustat, 43/58 [74.1%] PBO) completed 28 weeks of treatment, and 15 pts (6/82 [7.3%] roxadustat, 9/58 [15.5%] PBO) were continuing treatment. Median (range) treatment duration was 24.1 (1.1-28.0) weeks for the roxadustat arm and 28.0 (0.1-28.0) weeks for the PBO arm.
A greater percentage of pts in the roxadustat arm compared with the PBO arm were TI responders (47.5% vs. 33.3%). However, this difference did not reach statistical significance ( p=0.22; figure). Percentages of pts with TEAEs of any grade, serious TEAEs, and TEAEs leading to treatment discontinuation were similar across arms (table). Six deaths occurred on study (roxadustat: pneumonia [n=2], acute myocardial infarction and ischemic stroke [n=1], multiorgan failure [n=1]; PBO: urosepsis [n=1], disease progression [n=1]). Three pts (all in roxadustat arm) progressed to acute myeloid leukemia.
The study was terminated by the sponsor and is currently being completed.
Conclusions: Despite not meeting the primary endpoint, roxadustat plus BSC was well-tolerated, and a high percentage of pts with LR-MDS and LTB were TI responders. The high TI response rate in the PBO arm, historically poor outcomes in pts with ESA-refractory disease, and the inclusion of pts who were not transfusion-dependent (1 pRBC unit Q8W) may have contributed to the lack of a statistically significant difference in TI response rates between arms. MATTERHORN outcomes highlight the continued unmet need for effective and safe therapies that reduce RBC transfusion burden in LR-MDS.
Disclosures
Mittelman:Silence: Other: advisory boards; Astellas: Other: advisory boards; Janssen: Research Funding; Onconova: Other: advisory boards; Roche: Research Funding; Medison/Amgen: Research Funding; Novartis: Other: participated in clinical trials, advisory boards, Research Funding, Speakers Bureau; Celgene/BMS: Other: participated in clinical trials, Research Funding, Speakers Bureau; MDS HUB: Consultancy; Media Digital: Speakers Bureau; Geron: Other: participated in clinical trials; FibroGen: Other: participated in clinical trials; Takeda: Other: participated in clinical trials, advisory boards; Gilead: Consultancy, Research Funding; AbbVie: Other: participated in clinical trials, Research Funding. Henry:FibroGen: Research Funding. Glaspy:FibroGen: Research Funding. Tombak:GSK: Other: institution received research funding; Dr. Reddy's: Other: institution received research funding; BeiGene: Other: institution received research funding; FibroGen: Other: institution received research funding. Harrup:F. Hoffmann-La Roche Ltd, Beigene: Research Funding; F. Hoffmann-La Roche Ltd, Takeda: Current equity holder in publicly-traded company; FibroGen: Research Funding. Madry:AbbVie: Other: advisory boards, lecture fees; BMS: Other: advisory boards, lecture fees; Teva: Other: lecture fees. Grabowska:FibroGen: Research Funding. Platzbecker:Jazz: Consultancy, Honoraria, Research Funding; Servier: Consultancy, Honoraria, Research Funding; Syros: Consultancy, Honoraria, Research Funding; Geron: Consultancy, Research Funding; Merck: Research Funding; Janssen Biotech: Consultancy, Research Funding; AbbVie: Consultancy; Bristol Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel support; medical writing support, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Curis: Consultancy, Research Funding; MDS Foundation: Membership on an entity's Board of Directors or advisory committees; Silence Therapeutics: Consultancy, Honoraria, Research Funding; Fibrogen: Research Funding; Amgen: Consultancy, Research Funding; Roche: Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Celgene: Honoraria; BeiGene: Research Funding; BMS: Research Funding. Lee:FibroGen, Inc.: Current Employment, Current holder of stock options in a privately-held company, Other: stock. Modelska:FibroGen, Inc.: Current Employment, Current holder of stock options in a privately-held company, Other: stock.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal